What to expect on this page?
Sexually transmitted diseases (STDs) are infections acquired from another person mainly through the pathway of sexual activity. STDs are very common and put a heavy burden on public health in many countries. Luckily, these disease are treatable, some of them are curable, and, most important, all of them are preventable.
In the United States, about 20 million new sexually transmitted infections occur every year. That means that on average, an American has a 6% annual probability of getting an STD. Of course, an individual's chance of getting an STD depends on many factors, and homosexual intercourse is a major risk factor.
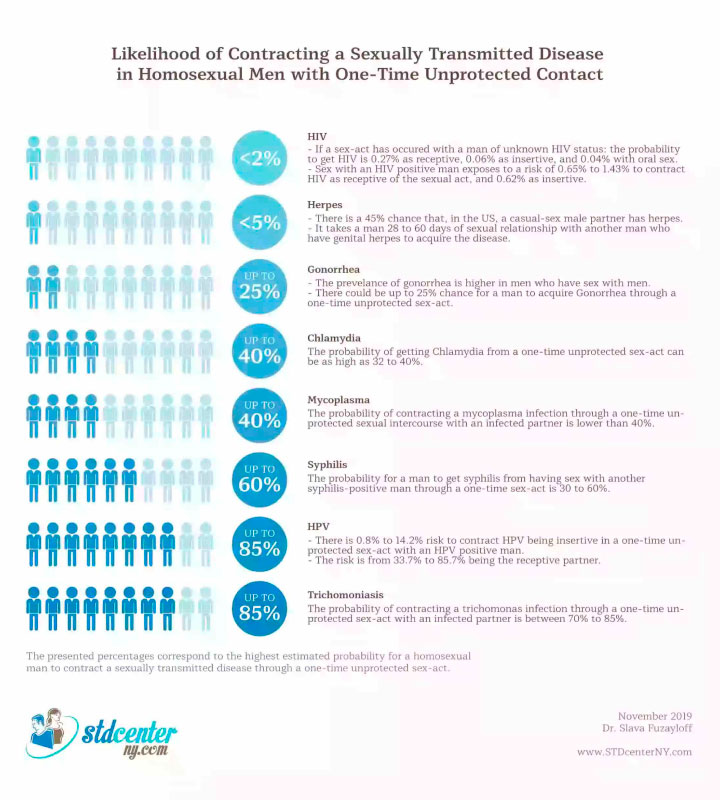
In this article, you will learn about the risks of contracting various STDs that homosexual males face when they have casual unprotected sex with other males.
We discuss the available data about these risks with respect to the following STDs:
- HIV
- Herpes
- Chlamydia
- Gonorrhea
- Syphilis
- Ureaplasma
- Mycoplasma
- Trichomoniasis
- HPV
HIV in homosexual men by the numbers
General overview
While other STDs, such as chlamydia and gonorrhea, are much more common, HIV is by far the deadliest. In the United States, the number of deaths attributed to HIV in 2017 was 34 times higher than the number of deaths attributed to all other STDs combined. Engaging in casual sexual activity exposes a person to HIV infection because some of those who carry the virus are not aware of their HIV-positive status and some HIV-positive individuals engage in unprotected sex without admitting that they have HIV. The risk of contracting the disease through casual sex is very hard to estimate because it depends on many variables that cannot be measured accurately, such as the number of sex acts, their timing, and other co-factors.
In general, the risk depends mainly on the prevalence of the disease in the region where the person is engaged in casual sex activity. For example, the general risk of contracting HIV from casual sex is 21 times higher in the District of Columbia, which has 46.3 HIV-positive persons per 100,000 population, than in Maine, where the prevalence is 2.2 per 100,000. And the risk is much higher in males who have sex with other males (MSM), who constituted 64% of people living with HIV in the United States in 2012. Four to seven percent of these people are unaware of their HIV-positive status. Because of this high variability, the risk of contracting an STD by having sex with a person whose status with respect to that STD is not commonly reported in the literature.
The risk of contracting HIV through one-time contact with a person of unknown HIV status
In an American study of MSM from 1992 to 1994, it was found that the general risk of contracting HIV through having sex with another man of unknown status is about 0.27% for the male receiving anal intercourse without a condom and 0.06% for the male who is the insertive partner in anal intercourse without a condom. The use of a condom reduces the risk to 0.18% for the receiver and 0.04% for the insertive partner. A receiver of oral ejaculation had a 0.04% risk of contracting the disease. These probabilities might be higher today because the prevalence of the disease has increased. While nowadays a higher proportion of HIV-positive people are on highly active antiretroviral therapy (HAART), which is known to reduce HIV transmission in heterosexuals, the male-to-male HIV transmission risk is not lower now than it was before HAART.
The risk of contracting HIV through one-time contact with an HIV-positive person
The probability of a male contracting the disease through unprotected anal sex with an HIV-positive male was estimated at about 1.43% if ejaculation had occurred inside the rectum and 0.65% if withdrawal occurred before ejaculation. The probability of an uncircumcised male contracting the disease through insertive unprotected anal intercourse with an HIV-positive male is 0.62%. Circumcision reduces this probability by more than 5 times but the existence of a genital herpes infection in either partner triples the probability.
The risk of contracting herpes for MSM
General overview
Herpes is caused by the herpes simplex virus (HSV) and is transmitted via skin-to-skin contact. HSV-1 causes orofacial and genital infections. HSV-2 causes primarily genital infections. However, each type may cause infections in either area, with HSV-1 implicated in up to 78% of anogenital lesions. In the United States, HSV-1 is more prevalent than HSV-2, though HSV-2 is predominant among African Americans and women. HSV-1 tends to be less symptomatic, which increases the risk of a sexual partner being a carrier and a transmitter of the disease without having a visible sore. In fact, most herpes transmissions occur through sex that occurred while the virus was not manifesting clinically (that is, there were no visible sores).
The probability of contracting herpes through homosexual contact
We did not ?nd speci?c numbers regarding the probability of a male acquiring genital herpes through sex with another male whose herpes status is unknown. In general, as with HIV, this depends on the prevalence of genital herpes in the region. In the United States, it was estimated in 2015-2016 that about 45.2% of males carry HSV-1 and about 8.2% carry HSV-2. That means that there is a 45.2% chance in the United States of a casual-sex male partner having HSV-1 and an 8.2% chance of him having HSV-2.
Furthermore, the real probability of contracting herpes from a person who carries it depends on the viral load at the moment of contact-which is impossible to measure. Very few studies directly used probability to measure the risk of acquiring herpes from a one-time sex-act. We did not ?nd any studies of male-to-male transmission that reported per-sex-act probability. The probability of an uncircumcised male acquiring herpes from a female was estimated to be between 0.3% and 0.7% per unprotected sexual act. As a better measure of this risk, Wald et al. proposed the median time that the relationship lasted before the acquisition of the disease. It was found that it takes a man, in a sexual relationship with a woman who has genital herpes, 120 days to acquire HSV-2 and 92 days to acquire HSV-1. In contrast, it takes a man in a sexual relationship with another man who has genital herpes only 28 days to acquire HSV-2 and 60 days to acquire HSV-1. Circumcision was found to cut these probabilities in half.
The risk of contracting chlamydia for MSM
Chlamydia trachomatis, a sexually transmitted bacterium, is the most commonly reported infection in the United States.
Speci?c data on the probability of getting a chlamydia infection after a casual one-time sex act is not available. This probability depends on the local prevalence of the disease, among other factors. It is estimated that about 1.4% of all males in the United States are infected with chlamydia. The prevalence is higher among those between 18 and 26 years of age-4.2%.
The transmission probability for heterosexual relationships has been estimated at about 68% when one partner carries the disease. This probability was similar for female-to-male and male-to-female transmission, suggesting that the transmission probability would likely be about the same for males having sex with other males. Another study converted this transmission rate to a time interval and estimated the probability at 4.5%. However, another study of the same subject estimated that the probability of transmission through a one-time sex act is as high as 32% to 40%.
The risk of contracting gonorrhea for MSM
Gonorrhea is the second-most-often-reported sexually transmitted disease in the United States, behind Chlamydia, with an estimated incidence of 600,000 new cases every year. Males who have sex with males have higher-than-average rates of gonorrhea, in general: 15.8%. Data on the probability of male-to-male transmission of the disease when the partner's gonorrhea status is unknown and when the partner is gonorrhea-positive are lacking. The most relevant data we could ?nd is that the probability of a man contracting gonorrhea by having a single-act unprotected sex with a female carrying the disease is estimated to be about 25%.
The risk of contracting syphilis for MSM
Syphilis is an infection caused by the bacterium Treponema pallidum. Transmission usually occurs via direct contact with an infectious lesion during sex; it can happen through vaginal, anal, or oral sex.
The probability of contracting syphilis is in general a function of the prevalence of the disease in the region. The number of new cases of syphilis in the United States is increasing; there were a record 35,063 new cases of primary and secondary syphilis in 2018. Primary and secondary syphilis are the most transmissible stages of the disease. Sixty-four percent of these cases were among MSM. The transmission probability does not seem to be very different for a heterosexual act and homosexual act. However, MSM, especially those between 15 and 40 years of age, are at higher risk of contracting the disease; the numbers show that this category is the one contributing most to new cases. Also, many males who get syphilis don't have any symptoms for years. The prevalence of syphilis among MSM in the United States has been estimated at 0.1%.
The probability of a male contracting syphilis through a one-time sex act with a syphilis-positive male is 30% to 60%.
The risk of contracting ureaplasma for MSM
Ureaplasma urealyticum is an emerging sexually transmitted disease that most commonly causes nonchlamydial nongonococcal urethritis in men but can also cause non-genital infections. The organism is also incriminated in male infertility. The infection can be transmitted through genital-to-genital or oral-to-genital contact. Data on the transmission rate of the infection was not found.
The risk of contracting mycoplasma for MSM
Mycoplasma genitalium is an emerging sexually transmitted bacterial infection with an increasing resistance to antibiotics. Transmission is primarily by genital-genital and penile-anal contact. Transmission through oral sex is unlikely.
The risk of contracting the infection through casual sex with a partner of unknown disease status depends on the prevalence of the disease in the region. The prevalence of Mycoplasma genitalium infection in the general population ranges from 1% to 2%. The infection is less prevalent in men but more prevalent in those who have multiple sexual partners.
It is not known what the average rate of transmission per episode of unprotected sexual intercourse is. However, it has been estimated that the probability of contracting a mycoplasma infection through unprotected sexual intercourse with an infected partner is lower than 40%.
The risk of contracting trichomoniasis for MSM
Trichomoniasis is a genitourinary infection caused by the parasite Trichomonas vaginalis
It's one of the most common sexually transmitted diseases in the world. The parasite tends to be carried by women more than men, but it is so common that its prevalence in men is also high. It is estimated that 0.5% of males in the United States carry the disease. Those who attend STD clinics tend to have higher rates of the disease, but MSM are not more likely to have this disease.
We could not ?nd speci?c data on male-to-male per-act probability of contracting the disease. H'owever, the disease has very high rates of infectivity in heterosexual relations, and if a male homosexual partner is a carrier of the infection, the transmission probability should be about the same. Considering also that male-to-female transmission rates are higher than female-to-male rates, the probability of contracting a trichomonas infection through a single act of unprotected sexual intercourse with an infected partner is between 70% to 85%.
The risk of contracting HPV for MSM
HPV is one of the most common sexually transmitted infections in the United States, accounting for more than one-third of new cases of STDs each year. About 70% of sexually active people acquire the infection at some point during their lives.
The prevalence of the disease is estimated to be very high in the United States, with about 15% of all US adults carrying it. The prevalence is about the same in males and females. It is estimated that up to 57% of MSM in the United States have anal HPV. Therefore, the probability of a male contracting the disease through having sex with another male of unknown HPV status is likely to be about half of what it is when the partner is known to be HPV-positive.
Estimated probabilities of HPV transmission from the penis to the anus are signi?cantly higher than those for transmission from the anus to the penis.
The probability of an insertive male contracting the disease through a single act of unprotected sex with an HPV-positive receptive male was estimated to be from 0.8% to 14.2%, depending on the HPV type in question.
The probability of a receptive male contracting the disease through a single act of unprotected sex with an HPV-positive insertive male was estimated to be from 33.7% to 85.7%, depending on the HPV type in question.
References
1. Shannon C, Klausner J. The Growing Epidemic of Sexually Transmitted Infections in Adolescents: A Neglected Population. Curr Opin Pediatr. 2018;30(1):137-143. doi:10.1097/MOP.0000000000000578
2. GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet Lond Engl. 2018;392(10159):1736-1788. doi:10.1016/S0140-6736(18)32203-7
3. Powers KA, Poole C, Pettifor AE, Cohen MS. Rethinking the heterosexual infectivity of HIV-1: a systematic review and meta-analysis. Lancet Infect Dis. 2008;8(9):553-563. doi:10.1016/S1473-3099(08)70156-7
4. Centers for Disease Control and Prevention. HIV in the United States by Region. Centers for Disease Control and Prevention. Published September 26, 2019. Accessed October 9, 2019.
5. Centers for Disease Control and Prevention (CDC). HIV testing and risk behaviors among gay, bisexual, and other men who have sex with men - United States. MMWR Morb Mortal Wkly Rep. 2013;62(47):958-962.
6. Vittinghoff E, Douglas J, Judson F, McKirnan D, MacQueen K, Buchbinder SP. Per-contact risk of human immunodeficiency virus transmission between male sexual partners. Am J Epidemiol. 1999;150(3):306-311. doi:10.1093/oxfordjournals.aje.a010003
7. Jin F, Jansson J, Law M, et al. Per-contact probability of HIV transmission in homosexual men in Sydney in the era of HAART. AIDS Lond Engl. 2010;24(6):907-913. doi:10.1097/QAD.0b013e3283372d90
8. Mahiane S-G, Legeai C, Taljaard D, et al. Transmission probabilities of HIV and herpes simplex virus type 2, effect of male circumcision and interaction: a longitudinal study in a township of South Africa. AIDS Lond Engl. 2009;23(3):377-383.
9. Mertz KJ, Trees D, Levine WC, et al. Etiology of genital ulcers and prevalence of human immunodeficiency virus coinfection in 10 US cities. The Genital Ulcer Disease Surveillance Group. J Infect Dis. 1998;178(6):1795-1798. doi:10.1086/314502
10. Mertz GJ, Coombs RW, Ashley R, et al. Transmission of genital herpes in couples with one symptomatic and one asymptomatic partner: a prospective study. J Infect Dis. 1988;157(6):1169-1177. doi:10.1093/infdis/157.6.1169
11. McQuillan G, Kruszon-Moran D, Flagg EW, Paulose-Ram R. Prevalence of Herpes Simplex Virus Type 1 and Type 2 in Persons Aged 14-49: United States, 2015-2016. NCHS Data Brief. 2018;(304):1-8.
12. Schiffer JT, Mayer BT, Fong Y, Swan DA, Wald A. Herpes simplex virus-2 transmission probability estimates based on quantity of viral shedding. J R Soc Interface. 2014;11(95):20140160. doi:10.1098/rsif.2014.0160
13. Magaret AS, Mujugira A, Hughes JP, et al. Effect of Condom Use on Per-act HSV-2 Transmission Risk in HIV-1, HSV-2-discordant Couples. Clin Infect Dis. 2016;62(4):456-461. doi:10.1093/cid/civ908
14. Wald A, Krantz E, Selke S, Lairson E, Morrow RA, Zeh J. Knowledge of Partners' Genital Herpes Protects against Herpes Simplex Virus Type 2 Acquisition. J Infect Dis. 2006;194(1):42-52. doi:10.1086/504717
15. Miller WC, Zenilman JM. Epidemiology of chlamydial infection, gonorrhea, and trichomoniasis in the United States--2005. Infect Dis Clin North Am. 2005;19(2):281-296. doi:10.1016/j.idc.2005.04.001
16. Quinn TC, Gaydos C, Shepherd M, et al. Epidemiologic and microbiologic correlates of Chlamydia trachomatis infection in sexual partnerships. JAMA. 1996;276(21):1737-1742.
17. Althaus C, Low N. Towards more robust estimates of the per sex act transmission probability of Chlamydia trachomatis. Sex Transm Infect. 2011;87(Suppl 1):A175-A175. doi:10.1136/sextrans-2011-050108.180
18. Katz BP. Estimating transmission probabilities for chlamydial infection. Stat Med. 1992;11(5):565-577. doi:10.1002/sim.4780110502
19. Little JW. Gonorrhea: Update. Oral Surg Oral Med Oral Pathol Oral Radiol Endodontology. 2006;101(2):137-143. doi:10.1016/j.tripleo.2005.05.077
20. Gunn RA, O'Brien CJ, Lee MA, Gilchick RA. Gonorrhea screening among men who have sex with men: value of multiple anatomic site testing, San Diego, California, 1997-2003. Sex Transm Dis. 2008;35(10):845-848. doi:10.1097/OLQ.0b013e318177ec70
21. Potterat JJ, Rothenberg RB, Woodhouse DE, Muth JB, Pratts CI, Fogle JS. Gonorrhea as a social disease. Sex Transm Dis. 1985;12(1):25-32. doi:10.1097/00007435-198501000-00006
22. Centers for Disease Control and Prevention. Syphilis - CDC Fact Sheet. Centers for Disease Control and Prevention. Published September 23, 2019. Accessed October 10, 2019.
23. Schober PC, Gabriel G, White P, Felton WF, Thin RN. How infectious is syphilis? Br J Vener Dis. 1983;59(4):217-219. doi:10.1136/sti.59.4.217
24. Gunn RA, Lee M, Oh C, Brodine S. Syphilis serologic prevalence monitoring among STD clinic clients: correlation with reported syphilis incidence, San Diego, CA, 1985-2004. Sex Transm Dis. 2007;34(10):749-753. doi:10.1097/01.olq.0000260916.69544.fe
25. Garnett GP, Aral SO, Hoyle DV, Cates W, Anderson RM. The natural history of syphilis. Implications for the transmission dynamics and control of infection. Sex Transm Dis. 1997;24(4):185-200. doi:10.1097/00007435-199704000-00002
26. Hook EW, Marra CM. Acquired Syphilis in Adults. N Engl J Med. 1992;326(16):1060-1069. doi:10.1056/NEJM199204163261606
27. Huang C, Zhu HL, Xu KR, Wang SY, Fan LQ, Zhu WB. Mycoplasma and ureaplasma infection and male infertility: a systematic review and meta-analysis. Andrology. 2015;3(5):809-816. doi:10.1111/andr.12078
28. Soni S, Horner P, Rayment M, et al. 2018 BASHH UK national guideline for the management of infection with Mycoplasma genitalium. :27.
29. Taylor-Robinson D, Jensen JS. Mycoplasma genitalium: from Chrysalis to multicolored butterfly. Clin Microbiol Rev. 2011;24(3):498-514. doi:10.1128/CMR.00006-11
30. Horner PJ, Martin DH. Mycoplasma genitalium Infection in Men. J Infect Dis. 2017;216(suppl_2):S396-S405. doi:10.1093/infdis/jix145
31. Patel EU, Gaydos CA, Packman ZR, Quinn TC, Tobian AAR. Prevalence and Correlates of Trichomonas vaginalis Infection Among Men and Women in the United States. Clin Infect Dis Off Publ Infect Dis Soc Am. 2018;67(2):211-217. doi:10.1093/cid/ciy079
32. Kelley CF, Rosenberg ES, O'Hara BM, Sanchez T, del Rio C, Sullivan PS. Prevalence of Urethral Trichomonas vaginalis in Black and White Men Who Have Sex With Men. Sex Transm Dis. 2012;39(9):739. doi:10.1097/OLQ.0b013e318264248b
33. Soper D. Trichomoniasis: under control or undercontrolled? Am J Obstet Gynecol. 2004;190(1):281-290. doi:10.1016/j.ajog.2003.08.023
34. Nelson AL, Woodward JA, eds. Sexually Transmitted Diseases: A Practical Guide for Primary Care. 2007 edition. Totowa, N.J: Humana Press; 2007.
35. Chin-Hong PV, Vittinghoff E, Cranston RD, et al. Age-Specific prevalence of anal human papillomavirus infection in HIV-negative sexually active men who have sex with men: the EXPLORE study. J Infect Dis. 2004;190(12):2070-2076. doi:10.1086/425906
36. Goldstone S, Palefsky JM, Giuliano AR, et al. Prevalence of and Risk Factors for Human Papillomavirus (HPV) Infection Among HIV-Seronegative Men Who Have Sex With Men. J Infect Dis. 2011;203(1):66-74. doi:10.1093/infdis/jiq016
37. Zou H, Tabrizi SN, Grulich AE, et al. Site-specific human papillomavirus infection in adolescent men who have sex with men (HYPER): an observational cohort study. Lancet Infect Dis. 2015;15(1):65-73. doi:10.1016/S1473-3099(14)70994-6